A dropped coffee mug. A blinding headache. A stumble on the stairs.
You could just be having a bad day. Or you could be having a stroke.
Would you know the difference?
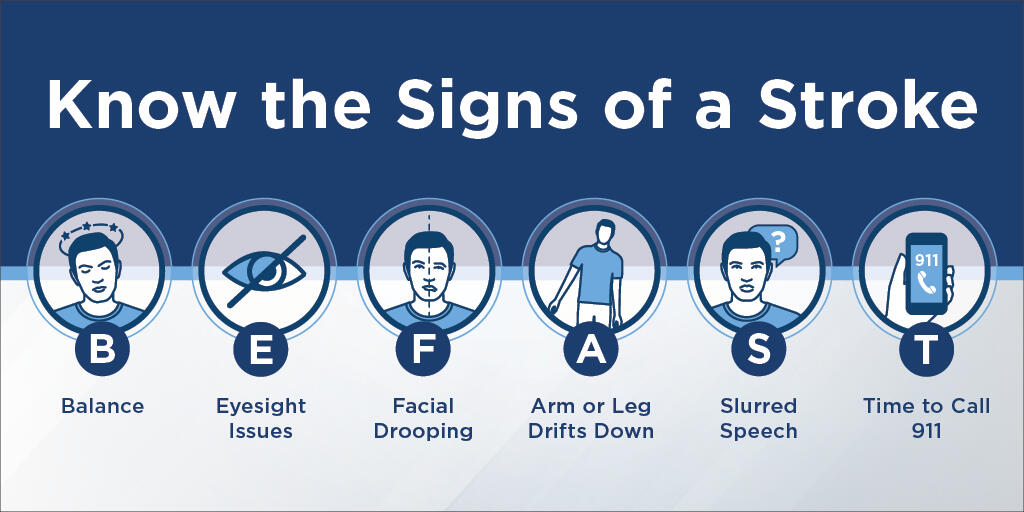
Learn the symptoms of a stroke using the BE FAST method.
A stroke happens when blood flow to an area of the brain is cut off. Brain cells are deprived of oxygen and begin to die.
Someone in the United States has a stroke every 40 seconds. And every four minutes, someone dies of a stroke.
With a quick response, you can survive a stroke
During a stroke, up to two million brain cells can die every minute, increasing your risk of permanent brain damage, disability or death.
If you are unsure of your symptoms, ask someone if they notice anything different about you. The effects of a stroke may cloud your ability to think and reason.
If you think you might be having a stroke, get help immediately!
If you are unable to call 911 yourself, have someone do it for you.
When you call 911, only describe what you feel and observe. Don't try to diagnose your problem.
When you arrive at the hospital, your healthcare team will assess your symptoms through a series of questions and tests. During the assessment, a detailed history will be taken and your speech, use of extremities and mental functioning will be observed.
Depending on the facility and the severity of your symptoms, you may undergo blood tests, a CT scan or other tests to help determine the cause. You may also be given medication, but that, too, will depend on the severity and type of stroke you are having.
If your symptoms are severe enough, you may be hospitalized. If the symptoms are mild, you may be sent home, with follow-up appointments or outpatient therapy treatment scheduled if needed.
Your recovery
The ability to recover from a stroke can vary greatly, depending on the type of stroke, the location of the stroke and the severity of the stroke.
Learn the types of stroke:
- Ischemic stroke: occurs when arteries are blocked by blood clots or by the gradual build-up of plaque and other fatty deposits. Ischemic strokes account for about 87 percent of all strokes.
- Hemorrhagic stroke: occurs when a blood vessel in the brain breaks, causing blood to leak into the brain. While hemorrhagic accounts for 13 percent of all strokes, they are responsible for more than 30 percent of all stroke deaths.
- Transient ischemic attack (TIA): Also known as a "mini-stroke," a TIA happens when blood flow to part of the brain stops for a short period of time. Symptoms are similar to a stroke but last for only 24 hours or less. However, a TIA can be a precursor for an actual stroke and should not be ignored. Forty percent of those who have a TIA will have a stroke, with nearly half occurring within a few days of the TIA.
Depending on what part of the brain is affected, a stroke can cause you to have difficulties with speech, movement and memory. Treatment can include medications and therapy.
There are three main types of therapy: physical, occupational and speech.
- Physical therapy helps you to deal with the aspects of a stroke that affect your physical abilities, such as range of motion, muscle strength and coordination.
- Occupational therapy helps restore your abilities or teach alternative methods for self-care, such as dressing, bathing, eating and preparing meals. Occupational therapy can also help you deal with the emotional aspects of a stroke.
- Speech therapy helps with speech and language problems and can improve your ability to swallow.
The mental and emotional side effects of a stroke can be tough to handle — for both you and your loved ones. You or your family members may feel anger, guilt, frustration or sadness. Medication for depression or counseling can help you and your family members deal with the emotional aspects of a stroke.
Sometimes it is helpful to talk to others who have experienced a stroke. The National Stroke Association offers a help line to connect you with tools and resources to guide you through your recovery process, including information about support groups in your area.
Tips for daily life after a stroke
Recovering from a stroke can take weeks, months or even years. These tips can help you get the most out of your recovery and back to enjoying life.
- Therapy doesn’t stop in the therapy gym. Continue to work on your exercises at home.
- Keep your mind active by working on number puzzles, like Sudoku, and word games each day.
- Create checklists for daily tasks, such as your morning routine or bills to pay. Don’t be afraid to ask for help from family and friends. Communicate with them so they know what’s happening with your recovery and why.
- When you've recovered as much as you are going to — if there are no signs of improvement for two to three weeks — therapy can go from focusing on improvements to learning how to deal with issues brought on by stroke and learning how to perform some activities in different ways.
- Consider whether you can take care of the tasks of daily living. Can you dress yourself, cook, pay bills, do household maintenance, etc.? Will you have help? If you have no one close by to help, can you hire help, such as home care services?
- If you cannot live at home anymore, be sure to find a nursing home with a good restorative nursing program.
Questions to ask about restorative nursing programs:
"Restorative nursing is focused on not letting someone decline in their abilities," says Priscilla Bragg, RN, Clinical Care Leader for the Good Samaritan Society. "It can follow a therapy program or treatment, but is provided by nurses and not therapists. It’s a great way for the nurses to quickly identify whether a person is losing ground or getting better. It helps to keep the person as independent as possible.
"Many people just want someone to do things for them, and they think the nursing staff is being lazy or mean if they make them do things for themselves," Priscilla says. "They don’t realize that by doing things themselves, they get stronger. It’s important that they keep moving forward or, at the very least, they don’t decline."
Questions to ask about a nursing home's restorative nursing program include:
- What does your restorative nursing program look like?
- Is it offered daily?
- Do you have trained employees specifically to support this program?
- If I have been receiving therapy, is there communication between the therapy and restorative nursing staff?
- If I don’t need this now, but my condition changes, how do you determine when or if I'll need it later?
- How frequently do you assess an individual’s abilities?
- Do you offer a variety of program options to make it fun and enjoyable?
Have patience with yourself. Recovery takes time. You may not go back to the way you were before the stroke. But keep in mind that many times, it's possible to learn to do something in a different way.
The most important thing to remember is to never give up. The strongest medication you have is your brain. With a positive outlook, you will go further in your recovery.
For more information on stroke visit https://www.cdc.gov/stroke/facts.htm.



