Many of us have heard stories of people falling when they’re older and some of those stories didn’t have a good outcome. Falling can sometimes lead to injury and death.
But falling doesn’t have to be an inevitable part of aging. There are many strategies people can use to help prevent falls, starting with education and screenings.
Learning why falls happen is an important piece of the puzzle.
Causes of falls
As we reach our retirement years, there are many reasons why we might be at an increased risk of falling, including:
- Decreased muscle mass
- Diseases such as diabetes, heart disease or thyroid conditions
- Improper footwear
- Medications that cause dizziness or confusion
- Mild cognitive impairment or certain types of dementia
- Mood – feeling depressed or not feeling well
- Rushing to the bathroom due to incontinence or another condition
- Safety hazards in the home or the community
- Vision changes
“Any adult older than 65 – that’s really when we start to see the risk of falling increase,” says Amber Jansen, a physical therapist and supervisor of therapy and rehabilitation at Good Samaritan Society – Bloomfield in Bloomfield, Nebraska.
Consequences of falls
When a person falls, they risk suffering a head injury or bone fracture. Hospitalizations are common and sometimes injuries lead to death.
The National Council on Aging and the Centers for Disease Control say that one in four Americans age 65+ fall each year and 20% are injured. Every 20 minutes, an older adult dies as a result of a fall.
People who have fallen once are more likely to fall again.
“Sometimes that fear creates another risk factor and the risk keeps increasing, causing more and more issues with falls and balance,” Amber states.
Bloomfield resident Susan Wachter is someone who’s experienced a pelvic fracture.
“I was on the ladder decorating my Christmas tree and shouldn’t have been up there,” Susan says. “I was laid up for three months.”
The Society’s rehab therapy team helped her recover.
“I would advise anybody that’s thinking about physical therapy and they have doctor’s orders to go because they just do wonders for you,” says Susan. “A lot of the stuff that I’ve done after I graduated, there was no way I could have done most of it before I started doing physical therapy.”
Another Bloomfield resident, Pat Hilfiker, experienced a fall in previous years. She’s had knee surgery which means she isn’t able to get to her feet very easily.
“I was outside working and just not watching what I was doing. All of a sudden, you’re down and then it’s hard to get up,” says Pat.
Screening to prevent falls
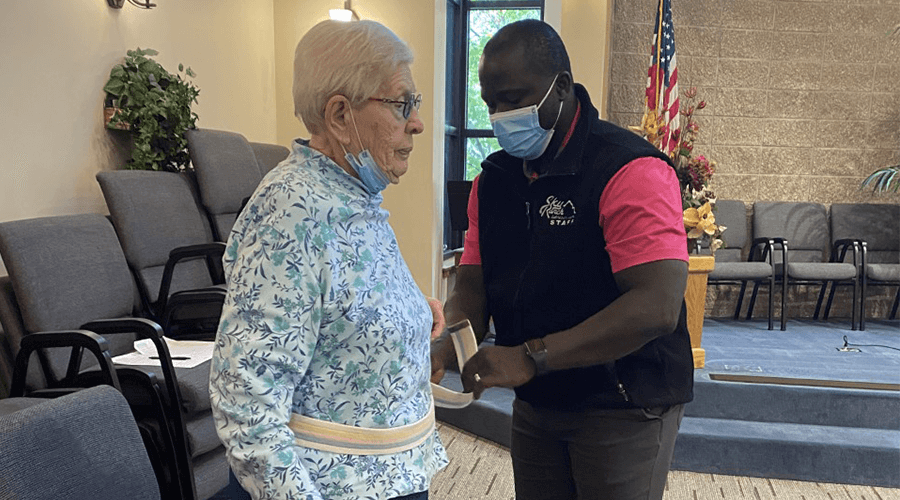
Screening events, like the ones held across the Good Samaritan Society, help seniors like Susan and Pat by educating them and assessing their risk so they can take proactive measures to prevent falls.
“Our screening events entail a self-reported falls risk form called the STEADI and also a screen by a therapist or a physical therapy assistant called the TUG – or timed up and go. Both of those are two really good screening options to help determine the risk level for a fall,” says Amber.
Participants are thankful for the assessments and the opportunity to learn more about taking care of themselves.
“They just remind you of things that you don’t think of every day,” says Pat. “This is my third year coming to the fall risk assessment and I’ve learned to wear decent shoes for one thing. Just being careful about watching what you’re doing, watching for loose things around the house and being careful when you have your pets running around.”
Amber’s recommendations for helping prevent falls include:
- Choosing good footwear (non-skid sole, less than a one-inch heel and laces that aren’t too loose)
- Eliminating rugs in your home
- Getting screened annually
- Rehab therapy or exercise to improve strength
- Using nightlights
“There are more complicated things that might require you to visit with your primary care provider about what kinds of medicines you’re taking,” says Amber.
At the Society’s screenings, therapy teams provide a comfortable environment where participants can ask questions.
“Sometimes we do see them in therapy afterward if they decide that it’s something they would like to pursue,” Amber states. “Or I’ll be told they were able to visit with their doctor and make some positive changes.”
Besides physical therapy, participants may be referred to occupational therapy to have a home safety assessment done.
“It’s a really good opportunity to get some ideas on how to make a home safer,” states Amber.